The Austrian-led retrospective review examined 15 consecutive, unselected patients with glioblastoma multiforme who received cannabidiol (CBD) in addition to standard treatment. Researchers found that overall survival was over “twice as long” as previously reported for standard treatment alone.
Despite being a relatively rare type of brain tumor, glioblastoma multiforme exhibits one of the lowest survival rates. Even with standard treatment which includes surgery followed by combined radiotherapy and chemotherapy, the median survival remains within 13.5 to 16 months after diagnosis.
The authors explained that two recent studies examining the overall survival of glioblastoma multiforme patients found that only 18% – 23.5% survive for two years and 10.3% – 11% survive for three years after diagnosis.
However, in the 15 patients observed by the Austrian team who were given CBD in addition to standard treatment, seven lived for at least two years (46.6% survival) and four of which for at least three years (26.7% survival).
“More than twice as long as has been previously reported in the literature,” the study authors said. Of all 15 patients, the average survival is currently 24.2 months, with 6 patients still alive today.
Is CBD an Effective Measure for Cancer?
Despite the small number of patients followed during in this retrospective review, the authors are encouraged by their findings.
“The low number of patients and the fact, that concomitant treatment with CBD was not subject of a clinical study may limit the generalization of our results,” the study authors said. “Nonetheless, overall survival is commonly considered as a hard endpoint.”
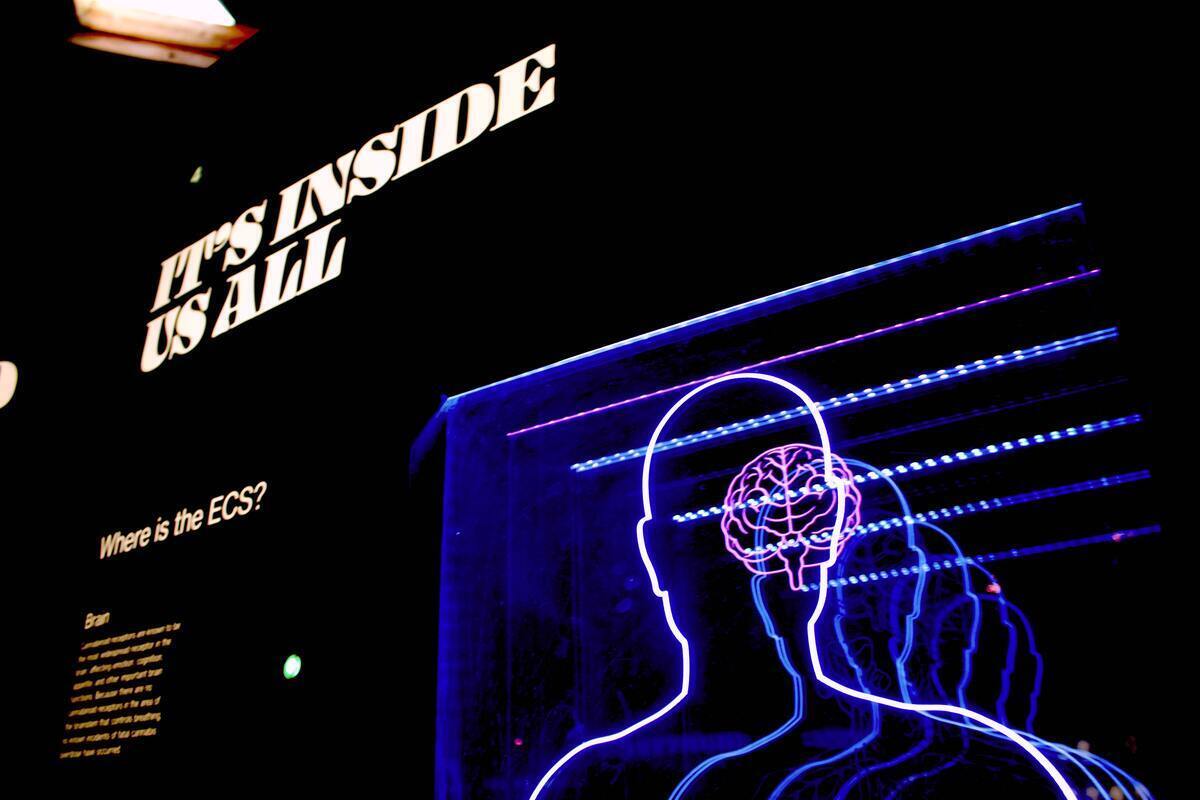
The authors explained that CBD has been shown to interact with over 8 different proteins involved in cancer development and progression.
Cannabinoids, particularly CBD, have also been shown in petri-dish and animal studies to block cancer cell growth in a wide range of tumors such as breast, cervix, colon, leukemia, lung, ovary, prostate, pancreas, and thyroid.
Similar studies in mice have found that CBD in combination with tetrahydrocannabinol (THC), another common cannabinoid, can effectively be used with existing chemotherapy to shrink glioblastoma tumor size.
In a recent 2021 phase 1b randomized and placebo-controlled trial using nabiximols, an oromucosal spray containing a blend of CBD and THC, researchers found that of the 12 glioblastoma patients taking nabiximols, ten survived for up to a year while only four of nine patients taking the placebo survived for the same period.
While these early studies suggest CBD can play a role in glioblastoma treatment, the authors explained that additional research is still needed to determine the mechanism by which CBD can eliminate cancer cells and determine an effective yet safe dosage for use.
Because the way cancer cells develop and operate can vary between types of brain cancer and even from patient to patient, the dosage and effectiveness of CBD in each case will likely vary as well.
“In conclusion, concomitant CBD seems to prolong the survival of patients with glioblastoma multiforme; CBD was well supported and did not cause side effects,” the study authors said. “Whether treatment with CBD could be optimized further by dose modulation and/or cannabinoid-combinations needs to be investigated.”